The World Health Organization (WHO) has officially declared the ongoing mpox outbreak in Africa a global health emergency. This is the highest level of alert under international health regulations. The announcement follows the public health emergency declaration made by the Africa Centres for Disease Control and Prevention (Africa CDC) on Tuesday.
Table of Contents

The World Health Organization (WHO) headquarters in Geneva, Switzerland on April 24, 2020.Fabrice Coffrini / AFP – Getty Images
Spread of a Deadlier Strain in Africa
A more lethal strain of the virus, clade Ib, has been spreading rapidly in the Democratic Republic of Congo (DRC) and has reached at least four other African countries previously unaffected by the outbreak. WHO Director-General Tedros Adhanom Ghebreyesus expressed concern over the potential for further international spread, calling it “very worrying.”
“It was unanimous that the current mpox outbreak is an extraordinary event,” stated Dimie Ogoina, chair of WHO’s emergency committee. “What we see in Africa is likely just the tip of the iceberg. We don’t have a complete picture of the mpox burden.”

World Health Organization (WHO) Director-General Tedros Adhanom Ghebreyesus speaks during a press conference on December 20, 2021 at the WHO headquarters in Geneva.
Fabrice Coffrini/AFP/Getty Images
Understanding Mpox
Mpox, previously known as monkeypox, is a viral disease related to smallpox, which has been eradicated. The virus can be transmitted through close contact, including touching, kissing, or sexual contact, as well as through contaminated materials like sheets, clothing, and needles, according to WHO.
The initial symptoms often resemble the flu, such as fever, chills, exhaustion, headache, and muscle weakness. These symptoms are usually followed by a painful or itchy rash with raised lesions that eventually scab over and heal within weeks.
What Makes This Outbreak Different?
The mpox virus is divided into two genetic clades, I and II. Clade II was responsible for a global outbreak declared a global health emergency from July 2022 to May 2023.
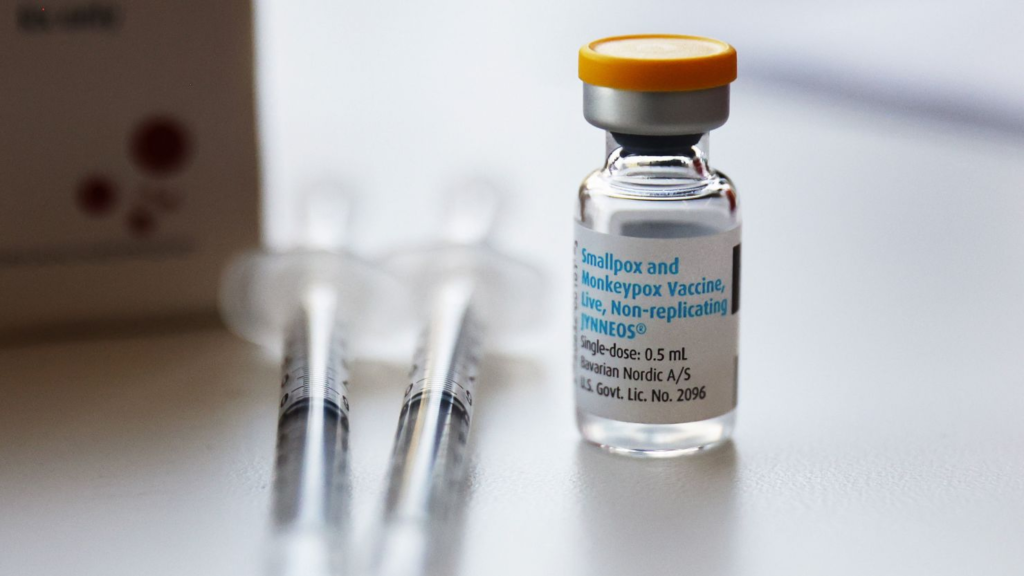
The Advisory Committee on Immunization Practices voted 14-0 on Wednesday to recommend people at high risk of mpox infection get two doses of the Jynneos vaccine.
Mario Tama/Getty Images
The current outbreak is driven by clade I, which causes more severe disease. The subtype clade Ib, which is relatively new, is primarily responsible for the ongoing spread.
“Clade Ib has emerged as a new mutation that is adapted to humans,” explained Dr. Daniel Bausch, a senior adviser for global health security at FIND, a nonprofit organization focused on health equity.
This mutation has allowed the virus, typically transmitted from animals to humans, to adapt and be transmitted between humans, leading to larger outbreaks.
The Danger of the Virus
Clade I mpox outbreaks have previously resulted in fatality rates as high as 10%, although more recent outbreaks have shown lower death rates, according to the US Centers for Disease Control and Prevention (CDC). The fatality rate for clade II is significantly lower, at less than 0.2%.
Certain groups, including infants, individuals with severely weakened immune systems, and pregnant women, are at higher risk of severe infection. However, surveillance of mpox is still incomplete, and much remains to be learned.
“This virus is present in the environment, likely maintained in small mammals in Africa, and our diagnostic capabilities are limited,” Bausch noted.
Geographic Spread and Current Concerns
For many years, mpox was primarily found in Central and West Africa. Clade I cases were mostly reported in Central Africa and the DRC, while clade II cases were largely confined to Nigeria.
However, in 2022, the virus began spreading to Europe and North America, raising global concerns.
The current outbreak is different from the one two years ago, as it is now affecting more countries in Africa that had previously been unaffected. While the majority of cases are still concentrated in the DRC, cases have been reported in at least 13 African countries, according to the Africa CDC.
On Thursday, Sweden reported its first case of clade I mpox, marking the first time the strain has been detected outside Africa.
Containing the Spread
While vaccines for mpox are available, they are not widely accessible in Africa. The US CDC has recommended vaccination for people in the US who are exposed to or at high risk of contracting mpox, although no cases of clade I have been identified in the country.
The Vaccine Alliance, known as Gavi, has allocated up to $500 million to supply mpox vaccines to affected countries, including the DRC. Gavi plans to establish a global stockpile of mpox vaccines by 2026, similar to its stockpiles for cholera, Ebola, meningitis, and yellow fever vaccines.
However, WHO emphasized that vaccines are only part of the response. Containing the spread will also require enhanced surveillance, diagnostics, and research to address gaps in understanding.
WHO has approved the Emergency Use Listing for mpox vaccines and developed a regional response plan requiring $15 million, with $1.5 million already released from the WHO Contingency Fund for Emergencies. Half a million doses of the vaccine are in stock, and another 2.4 million could potentially be produced by the end of the year. The DRC and Nigeria will be the first to receive these vaccines.

WHO Representative to Uganda gets COVID-19 vaccine jab. This was to build confidence in the vaccine in order for health workers and everyone eligible to get it.
You may also want too this article